Your menstrual cycle is more than just a monthly event; it is a direct reflection of your overall health and well-being. In both Traditional Chinese Medicine (TCM) and Western medicine, the menstrual cycle is considered a powerful diagnostic tool, offering insight into hormone balance, fertility, and long-term health risks. Yet many women are never taught to understand or track their cycles beyond managing symptoms. By paying closer attention to your menses, you can uncover valuable information about your body, optimize your reproductive health, and prepare for a smoother transition into menopause.
1. Your Health
Your menstrual cycle, or lack thereof, is a reflection of your overall health. This understanding is deeply rooted in centuries of TCM, but it also entered mainstream Western medicine when the American College of Obstetricians and Gynecologists (ACOG) published a Committee Opinion in 2006 (reaffirmed in 2015). ACOG recommends that clinicians treat menstrual history as a vital sign, alongside temperature, pulse, respiration, and blood pressure. Author Lisa Hendrickson-Jack further popularized this concept in her book The Fifth Vital Sign.
Yet despite these recommendations, menstrual disorders often remain underdiagnosed and neglected. A key reason is that menstrual cycle characteristics are not routinely assessed or documented in conventional clinical practice.
In my clinical experience, the menstrual cycle is an underutilized but powerful diagnostic tool for understanding gynecological and general health. Like a vital sign, it provides crucial information that can guide treatment plans, monitor symptom progression, and inform preventive care strategies. Research also shows that menstrual patterns can predict fertility outcomes, chronic disease risk, and even the timing and experience of menopause.
2. Fertility Outcomes
Many women are surprised when they do not conceive quickly or when underlying gynecological conditions emerge after coming off birth control. Often, they have been disconnected from their body’s natural rhythms, discouraged from understanding their cycles, or led to believe that menstrual symptoms are simply “part of being a woman.”
Reduced fertility is not just about reproductive health; it is a sign that something in the body is out of balance. These imbalances are unique to each individual and need to be identified before they can be corrected. Today, more women are trying to conceive later in life while managing demanding careers and home responsibilities. Many seek TCM only after multiple failed assisted reproductive cycles such as medicated intercourse, IUI, or IVF.
For years, women have suppressed menstrual symptoms through medication or by simply enduring them. This often means underlying health concerns remain unaddressed until conception becomes difficult.
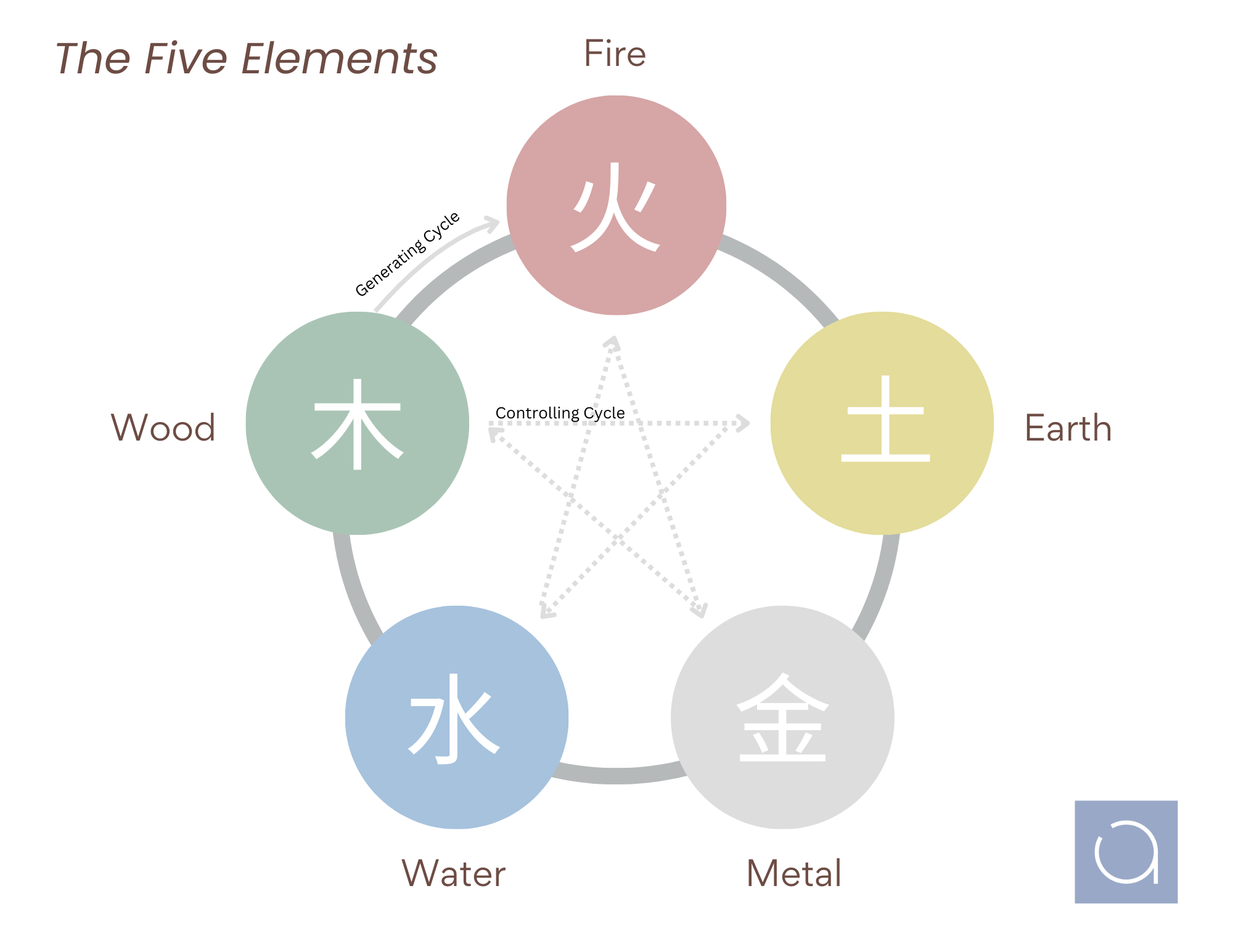
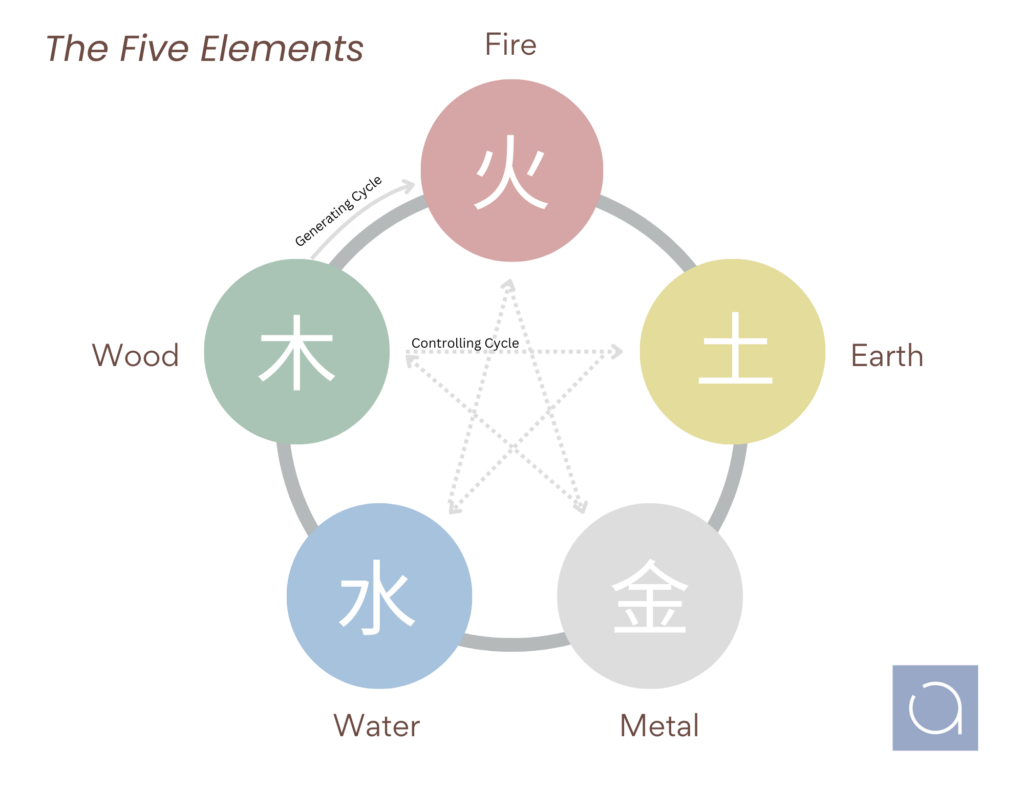
From a TCM perspective, menstrual disorders reveal how the body’s systems, including hormones, are functioning as a whole. For example:
- Digestive symptoms like bloating or irritable bowel issues may signal nutritional deficiencies affecting fertility.
- Feeling cold or experiencing chronic fatigue may point to thyroid imbalances, which can lead to infertility or pregnancy loss.
- Migraines and severe cramps may be tied to blood clotting or circulation issues, sometimes seen in women with recurrent miscarriages.
This is where Chinese medicine shines. Its diagnostic approach explores all aspects of health, including digestive, respiratory, cardiovascular, urinary, musculoskeletal, energy levels, body temperature regulation, sleep patterns, and more. While some findings may require conventional interventions, such as thyroid medication, TCM treatments aim to address root causes of imbalance, improving both general health and reproductive capacity.
3. Menopause
Menopause is not a disease. It is a natural transition from reproductive to non-reproductive years. Traditionally, women were not expected to experience disruptive symptoms during this stage of life. Medical support was considered necessary only when symptoms significantly affected quality of life.
Today, however, menopause has become a growing area of focus in healthcare and even the workplace. With longer lifespans and a rising global population of women entering midlife, there is increasing recognition of how menopause impacts physical health, emotional well-being, and career performance.
It is also worth noting that definitions of menopause have shifted. Historically, menopause was marked by 12 consecutive months without menstruation. Now, the transition is often identified earlier, as irregular cycles, hot flashes, and hormonal fluctuations appear. Around 75% of women experience hot flashes during this period, yet fewer than half seek treatment.
What is fascinating is that classical Chinese medical texts rarely focus on menopause as a condition. Instead, the emphasis was on gynecology and postpartum care, underlining the importance of maintaining balance throughout reproductive years.
Could better understanding and care of the menstrual cycle during youth and adulthood lead to fewer symptoms during menopause?
Conclusion
Your menstrual cycle tells an ongoing story about your health, from your first period to your fertility years and into menopause. By learning to interpret its signals, you can take proactive steps toward better balance and long-term well-being. Whether you are trying to conceive, manage hormonal changes, or simply want to feel more in tune with your body, understanding your menses is key. At Aetherium Acupuncture & Integrative Medicine, we help women uncover the deeper connections between their cycles and overall health through personalized Chinese medicine treatments, education, and holistic support.
References:
American Academy of Pediatrics. (2006). Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Pediatrics, 118(5), 2245–2250.
American College of Obstetricians and Gynecologists. (2015). ACOG Committee Opinion No. 651: Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Obstetrics & Gynecology, 126(6), e143–e146.
Maciocia, G. (n.d.). Obstetrics and gynecology in Chinese medicine (Kindle ed.). Elsevier Health Sciences.
Rosen Vollmar, A. K., Mahalingaiah, S., & Jukic, A. M. (2025). The menstrual cycle as a vital sign: A comprehensive review. F&S Reviews, 6, 100081. https://doi.org/10.1016/j.xfnr.2024.100081
Rosen Vollmar, A. K., Mahalingaiah, S., & Jukic, A. M. (n.d.). The menstrual cycle: A vital sign across the lifespan. The Lancet Obstetrics, Gynaecology, & Women’s Health, 0(0), 100001.
World Health Organization. (2024, October 16). Menopause fact sheet. https://www.who.int/news-room/fact-sheets/detail/menopause